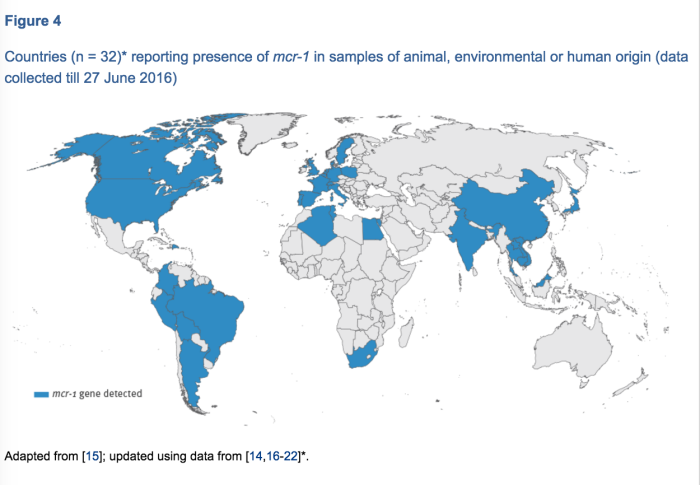
Recent identification of mcr-1, a gene that makes bacteria resistant to colistin (an antibiotic of last resort) raised a lot of concern. Now, there’s another one to be worried about, as a related gene, mcr-2 has been identified (Xavier et al, Eurosurveillance, July 2016).
In this study, 105 colistin-resistant E. coli from calves and piglets in Belgium were studied. mcr-1 was found in 12% of these. They then looked at 10 of the bacterial isolates that were colistin-resistant but negative for mcr-1. They found a new resistance gene related to mcr-1 (and not surprisingly named it mcr-2) in 3 of the isolates.
That’s bad enough.
Of additional concern is that the gene was found on plasmids, which are smaller pieces of DNA (separate from the bacteria’s chromosomal DNA) that can be transferred readily between bacteria. They found that mcr-2 had a 1200-fold higher transfer frequency compared to mcr-1 on its plasmid, meaning (under lab conditions, at least), that it’s much more adept at moving between bacteria. If it truly can more readily hop to other bacterial species (and therefore potentially more disease-causing bacteria), that’s even more concerning.
Does this mean that we’re seeing a rapid rise in colistin resistance genes?
Probably not. The bacteria from which mcr-2 was isolated were collected in 2011-2012. The increase in recent reports is most likely a factor of an exponential increase in people looking for colistin resistance in bacteria from animals and people. mcr-3 and 4 are probably lurking in the gut of a person or animal somewhere, they just haven’t been described yet.
Is this really a concern?
Yes. While the number of people that will be infected with bacteria possessing these genes will hopefully remain low, these raise the spectre of the “untreatable infections.” When your drug of last resort is gone, you’re in big trouble.
What do we need to do?
There’s no simple answer. A lot involves common sense, good infection control, infection prevention and prudent antibiotic use. These will help reduce the number of infections of any sort, and with fewer infections, along with less (and better) antibiotic use, the spread of resistance genes like this can likely be reduced. They’re not going to be eradicated, but if we can keep them contained, their impact can be lessened.
The authors’ conclusion: Taken together, these data call for immediate inclusion of mcr-2 screening in ongoing molecular epidemiological surveillance to gauge the worldwide dissemination of mcr-2 in both human and animal colistin-resistant Gram-negative bacteria of medical importance.
Figure from Xavier et al, Eurosurveillance 2016