Many countries have import requirements for dogs based on rabies control (among other things), primarily based on the dog’s rabies vaccination history, plus or minus rabies antibody titre (RAT) testing. A few years ago (with support from the Ontario Animal Health Network), we studied RATs in dogs imported into Ontario by rescues (Belanger et al. 2025). I also wrote a bit about this study last year when it was first published online. It wasn’t easy to recruit groups to participate, but we ultimately were able to test blood samples from 67 dogs. The results were… disappointing, and concerning, but not surprising.
Dogs were sampled at the time of arrival to Canada or shortly after (before any additional rabies vaccines were given), and blood samples were sent to Kansas State University for the rapid fluorescent focus inhibition test (RFFIT), which is the gold standard for RAT testing. The standard cutoff for an “acceptable” titre (demonstrating response to vaccination) is 0.5 IU/ml.
- 48% of these dogs had RATs less than 0.5 IU/ml.
- 19 (28%) had no detectable titre at all.
Rabies antibody titres had been test prior to shipping in 29 of these dogs, all of which came from Egypt. The Egyptian lab used an ELISA test to measure the titres 30-40 days after vaccination. While all 29 dogs had “adequate” titres based on the ELISA, only 11 (38%) had adequate titres when they arrived in Canada, based on the RFFIT. There was a median of 7 days between the pre- and post-import testing in these dogs, so it’s unlikely that a natural drop in antibody levels would account for the difference in testing. This raises questions about the accuracy of the pre-import testing in other countries, and highlights why countries that have RAT requirements for dogs are quite strict about what labs can perform this testing.
Close to 50% of imported dogs in this study had poor (or no) RATs. That’s a concern, especially considering this group may actually be better than than average, since they agreed to participate in the study (selection bias). We know some dogs get imported with false rabies vaccination documentation, and those using faking documents would be unlikely to volunteer to participate.
These results weren’t actually too surprising compared to other studies though. A study of dogs imported into Finland reported no detectable antibodies in 39% of dogs (Kaila et al. 2019). Another European study reported inadequate titres in 53% of imported dogs (Klevar et al. 2015).
Why did so many imported dogs have “inadequate” rabies titres, even though they all had to be vaccinated prior to arrival?
It’s hard to say. There are a few possible explanations:
- Poor vaccine response: Not all animals respond well to a vaccine, particularly a single dose. Rabies vaccine is a really good vaccine in this respect, but we know that not all dogs will respond well, even with the best vaccine. For example, a study of dogs less than 1 year of age in the US that received a single rabies vaccine showed that 12% of dogs failed to reach the 0.5 IU/ml RAT (at various time points, mostly within 6 months of vaccination) (Wallace et al 2017). A study of dogs in Sri Lanka showed that a single rabies vaccine failed to produce a titre of over 0.5 IU/ml in 40-57% of dogs a year after vaccination (Pimburage et al. 2017), which tells us about both the magnitude and duration of the antibody response. These studies suggest that we can’t necessarily count on good protection in all dogs (in some situations) after a single dose, but many of these dogs with poor titres may still respond well to a booster dose, which is why revaccination is critical.
- Vaccine quality and handling: Vaccine quality varies internationally, and perhaps more importantly, vaccine handling (maintaining cold chain) can play a role in whether a vaccine is effective or not. It’s possible that poor responses in some situations were from questionable or mishandled (and therefore ineffective) vaccine. In our study, 46% of the dogs were reportedly vaccinated abroad using a rabies vaccine licensed in Canada, but only 46% of those dogs had a titre of 0.5 IU/ml or higher on arrival. Using a Canadian licensed vaccine gives us confidence that it was high quality product when it was manufactured, but if there were handling issues (e.g. not kept cold), that could compromise vaccine efficacy.
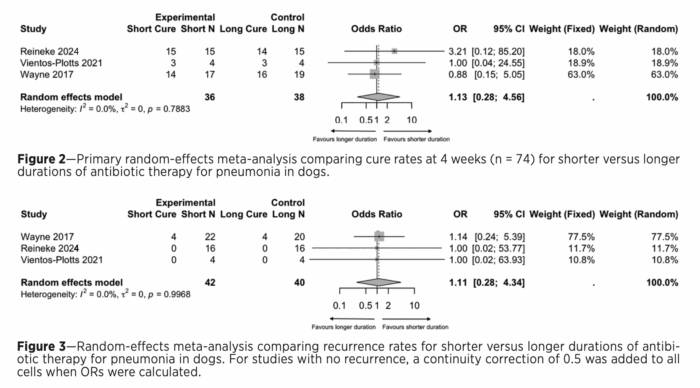
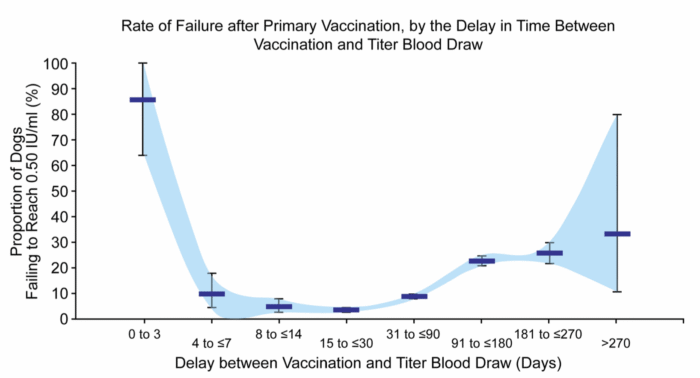
- They were vaccinated too soon before testing to detect titres: Vaccines stimulate the body to produce antibodies, but that’s not an instantaneous process. When a dog gets its first rabies vaccine, it can take a little while for antibodies to reach detectable levels, and then levels will rise for a short time. (With subsequent boosters, the response is much quicker). The median time from vaccination to sampling in our study was 42 days, which is lots of time to see the antibody response if it happens, but ranged as low as 3 days. It wouldn’t be surprising to find low or undetectable titres in a dog vaccinated for the first time 3 days earlier, but the vaccine response ramps up quickly, as shown in the graph below from the Wallace et al. 2017 paper. So, I doubt timing of testing played a significant part in most of the dogs with low titres.
- The dogs weren’t actually vaccinated: This is probably less likely in our study, since groups that falsify vaccination certificates are not likely to agree to participate. It’s a big concern in general, though, since falsified rabies vaccination certificates have been detected and are a recurrent issue.
Another relevant question involves the 0.5 IU/ml titre target, which is not considered “protective” because we don’t actually know what a true “protective titre” is. The cutoff we use basically inidcates that the dog has responded to a rabies vaccine. With that, it probably has some degree of protection and also has an immune system that is primed to pump out more antibodies in response to future exposure or vaccination. A dog with a titre less than 0.5 IU/ml might still have responded to the vaccine and could respond very well to a booster, but we have less confidence in its current status. Dogs with a zero titre are more of a concern since that doesn’t give us any evidence that they have been vaccinated at all or had any form of response to a vaccine. In short, a dog with a titre of 0.4 IU/ml is quite possibly fine, but a dog with a 0.0 IU/ml titre is at far greater risk.
So, what now?
We’re going to continue to import dogs and no import rules will be perfect (or perfectly followed). Trying to maximize rabies vaccination and use of good quality vaccine in imported dogs is key. Beyond that, giving a dog a rabies booster at the time of arrival is prudent – and also legally required in Ontario, if the dog was not vaccinated with a vaccine licensed in Canada or the US by a veterinarian licensed in Canada or the US.